Postgraduate Diploma in Community Geriatrics (Sunsetted)
社區老年醫學深造文憑
This well-established and clinically oriented advanced Course was first launched in the year 2000. It was the first of its kind in Hong Kong and aimed to upskill primary care doctors to provide medical care services to the senior citizens in the community while Hong Kong had become a rapidly ageing society.
The Course adopted a student-centred approach and multiple-mode of learning to maximise outcomes. Developed in conjunction with The Hong Kong Geriatrics Society, it used three different modes of study: distance learning, interactive workshops and clinical teaching. Students learned in small groups and were coached by senior and experienced geriatricians working in the public sector. A postgraduate diploma was awarded upon satisfactory performance in the Course assessment and final examinations.
A quotable qualification was granted to our graduates from the Medical Council of Hong Kong within three months of the completion of the first batch of students and before their formal graduation - a record at the time. The Course has bred graduates who have played important roles in geriatric care and made presentations at international geriatric conferences. Locally, it had been the only postgraduate diploma course that provided practising doctors with further training in geriatric medicine.
Owing to decreased enrollment numbers in recent years, our Department no longer offers admission to this Course which has therefore been sunsetted since 2018.
Features
- A Quotable Qualification by the Medical Council of Hong Kong
- Clinically Oriented
- Multiple Learning Modes
- Flexible Teaching Hours
- Clinical Teaching Sites across Hong Kong
Objectives
Background
Good health is central to an older person's enjoyment and satisfaction with later life, even when it has been taken for granted in younger years. Although the majority of senior citizens are well, many have chronic ailments and when illness does strike it can have a significant impact on the well-being and quality of later life. As a group, the senior citizens have the highest level of medical and social needs, and doctors are attending to more people from this group than in the past. It is anticipated that Hong Kong's elderly population reaches 1.4 million by 2020, while a large portion of our seniors are presently looked after by their primary care doctors in the community.
Prior to the launch of this Course, structured training opportunity in geriatric medicine for the practicing primary care doctors was practically non-existent. This Course, the first of its kind in Hong Kong, filled a long awaited and much welcome educational as well as social void, as reflected by a three-fold over-subscription in its first intake. Over 250 doctors had enrolled in this Course since its inception in 2000.
Objectives
- To promote good practice in geriatric medicine among primary care doctors
- To improve the knowledge, skills and confidence of practising doctors in the care of the elderly
- To present information on the medical care of senior citizens that is practical, concise, unique to this group and relevant to primary care
- To appreciate the interdisciplinary nature of geriatric medicine
- To focus on community care, i.e. assessment and treatment of senior citizens in their normal community environment, and the use of community resources as an integral part of their care
- To emphasise the importance of prevention and health maintenance among senior citizens
Structure & Content
Course Structure
| Written Component | Clinical Attachment | |
| Features | 10 weeks of distance learning study |
20 sessions of clinical geriatric
teaching
5 sessions of rehabilitation and community health services |
| 5 interactive workshops | ||
| Study Period | September - November | November - May in the following year |
| Time |
5 Saturday afternoons
2:30 - 5:15pm |
25 weekday
afternoons (2:00-4:00 pm) or evenings (6:30-8:30 pm) |
| Venue | LKS Faculty of Medicine, HKU | Public hospitals |
| Assessment | Written assignments, written examination and clinical examination | |
Distance Learning Study
A set of distance learning materials developed by the Hong Kong Geriatrics Society were distributed to students at the beginning of the Course. The materials contained both text and exercises to facilitate self-study at home. Students were required to complete 6 short assignments (based on the learning materials) within 10 weeks (by the end of December). Content of the learning manual covered the followings:
Geriatric Services and Approaches
- Community geriatric care and rehabilitation
- Use and abuse of drugs
- Interpretation of laboratory investigations
- Palliative care and pain management
- Ethical issues and communication skills
Geriatric Syndromes
- Falls and accidents
- Urinary incontinence and constipation
- Dementia and delirium
- Depression and anxiety
- Impaired vision and hearing and malnutrition
Common Geriatric Diseases
- Stroke
- Parkinsonism
- Musculoskeletal disorders
- Cardiovascular disorders
- Common skin problems
- Diabetes mellitus
Interactive Workshops
There were 5 Interactive Workshops held on Saturday afternoons (2:30-5:15 pm). Each workshop covered 2 topics and invited prominent geriatricians/family physicians to deliver talks and lead discussion.
*Topics for the Workshops:
- Introduction to geriatric medicine
- Geriatric services in Hong Kong and community geriatric care
- Ethical considerations and communication skills in the care of elderly people
- Dementia and delirium
- Falls and accidents in old age
- Urinary incontinence and constipation in old age
- Common dermatological problems in elderly people
- Use and abuse of drugs in old age
- Interpretation of laboratory investigations in elderly people
- Comprehensive geriatric and functional assessment of cognitive, language, visual and hearing impairment
* Topics might be revised.
Clinical Attachment
There were 25 clinical sessions held weekly from November to May the following year at designated public hospitals where the geriatric teams were based. Students were divided into small groups and attached to the teaching hospital of their choice. Each session lasted 2 hours and was led by a tutor (either senior medical officer or consultant from the hospital).
Content of the clinical sessions:
5 sessions on rehabilitation and community health services
- Day hospital: allied health services, physiotherapy, occupational therapy, speech therapy and podiatry
- Community geriatric assessment team and community nursing services
- Specialised clinical sessions
20 sessions of clinical geriatric teaching
- Stroke
- Palliative care in elderly
- Pressure sore
- Dementia / cognitive impairment
- DM in elderly - age related changes
- COPD : age related changes
- CHF/hypertension/cardiac arrhythmia
- Sensorium
- Rheumatological conditions (osteoporosis /hip/OA knees)
- Bladder dysfunction
- Depression/anxiety
- Instability with recurrent falls
- Parkinson disease
- Malnutrition
- Iatrogenesis and multiple pathology
- Social deprivation
- Acute confusion in elderly
Schedule and Venue
The Course commenced in September and finished in June the following year.
| Month | 9 | 10 | 11 | 12 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 |
| Distance learning | ||||||||||||
| Written assignments | ||||||||||||
| Interactive workshops | ||||||||||||
| Clinical attachment | ||||||||||||
| Examinations | ||||||||||||
Teaching sites:
| Study Mode | Venue |
| Distance learning | Self-study at home |
| Interactive workshops | Seminar Rooms, LKS Faculty of Medicine Building, 21 Sassoon Road, Pokfulam, Hong Kong |
| Clinical Attachment | Students were assigned to attach to one of the following five groups: HK, Kowloon 1, Kowloon 2, NT East and NT West. |
| Student Groups | Teaching Hospitals for clinical sessions |
| Hong Kong |
Ruttonjee Hospital
TWGHs Fung Yiu King Hospital |
| Kowloon 1 |
Caritas Medical Centre
Kwong Wah Hospital Princess Margaret Hospital |
| Kowloon 2 |
Kowloon Hospital
Our Lady of Maryknoll Hospital United Christian Hospital |
| NT East |
Alice Ho Miu Ling Nethersole Hospital
Shatin Hospital Tai Po Hospital |
| NT West |
Tuen Mun Hospital
Yan Chai Hospital |
Teaching Hours for clinical attachment*:
| Student Groups | Class Schedule |
| Kowloon 1, NT West | Weekday afternoons (2:00 - 4:00 pm) |
|
Hong Kong, Kowloon 2,
NT East |
Weekday evenings (6:30 - 8:30 pm)
(Up to 5 sessions might be held during office hours for availability of patients for demonstrations) |
* Students were required to attend at least 80% of all the clinical sessions in order to fulfill the requirements for the award of the diploma.
Assessment & Awards
Assessment
The performance in written assignments and clinical attachment provided continuous assessment. There were also final examinations held in June with a written paper (computer-based MC questions) and a clinical examination in the format of Objective Structured Clinical Examination (OSCE). Examiners comprised family physicians and geriatricians. Overseas external examiner was invited to participate in the final examinations.
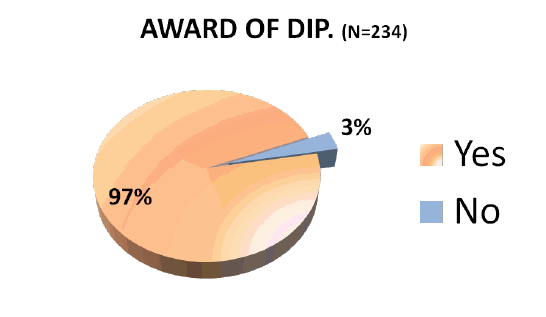
Award of Diploma
The Postgraduate Diploma in Community Geriatrics was awarded to the candidates who completed the whole Course and performed satisfactorily in the Course assessment and final examinations. The Diploma was recognised as a quotable qualification by the Medical Council of Hong Kong.
Accreditations for CME, CPD and SEP points were applied to the Colleges of the Hong Kong Academy of Medicine, Department of Health, Hong Kong Medical Association and Hong Kong Doctors Union.
Conjoint Clinical Examination Discontinued
A Conjoint Clinical Examination for the Postgraduate Diploma in Community Geriatrics (PDCG) and Diploma in Geriatric Medicine (DGM) of the Royal College of Physicians and Surgeons of Glasgow (RCPSG) had been launched since June 2008. However, as informed by the RCPSG on 31st March 2014, they had discontinued their provision of a Diploma in Geriatric Medicine (DGM). As a result, our Department no longer provided a conjoint clinical examination from April 2014 onwards.
Learning Outcomes
i. Learning Outcomes
Evaluative Study on Learning Outcomes of Postgraduate Diploma in Community Geriatrics
An evaluative study was carried out on the learning outcomes of the graduates in 2008 and a report on the findings was published in 2009. The study results were also published in an article entitled Evaluation of the learning outcomes of a year-long postgraduate training course in community geriatrics for primary care doctors in the
Background
There is an increasing worldwide trend to strengthen the quality of primary care doctors by further postgraduate stud ies. Although overseas experiences have indicated improvements in doctors' clinical practice and other areas after taking postgraduate courses, little is known about the possible effect of these courses in enabling doctors to handle cases which would reduce burden of specialists and their participation in more demanding community healthcare activities. The present study aims to fill the gap in this respect and has selected the Postgraduate Diploma in Community Geriatrics (PDCG) as its main subject. The PDCG, developed by the Family Medicine Unit of The University of Hong Kong in conjunction with the Hong Kong Geriatrics Society, has trained over 200 primary care doctors since 2001.
Aims
Methods
A questionnaire designed by the research team was sent to all graduates (2001-2007) of the PDCG between August and December 2008 after its pilot test in mid July of the same year . To enhance the response rate, three rounds of invitation were sent followed by telephone reminders. The questionnaire itself was anonymous but was coded with a reference number to identify the respondent for the lucky draw prizes or for deletion from the next round of invitation.
Results
Out of the 188 questionnaires sent to the graduates, 1 postal address was invalid. 98 replies were received with a response rate of 52.4% (98/187). Of the respondents, 7 8 . 6 % were male and 2 1.4 % female, 91.8% were in community practice while 8.2 % in hospital practice , 36.1 % were in public service and 63.9 % in private service . A great majority ( 91.8 % ) of the respondents were primary care doctor s, and the mean years after graduation from medical school was 14.6 ± 9.48.
The respondents rated the reasons for studying the Course in descending order of importance : 1) update clinical knowledge (100.0%), 2) improve care for the elders (99.0%), 3) lifelong learning (92.8%), 4) interest in community geriatrics (91.7%), 5) acquire qualifications (83.7%), 6) career enhancement (63.3%), 7) meet job demand (61.5%), and 8) CME accreditations (53.1%).
The rated major learning outcomes , in descending order of agree ment , were : 1) modification of approach to elderly patient care (95.9%), 2) felt more rewarding in geriatric care (84.7%), 3) participated more in geriatric care (82.7%), 4) improved communication skills with elderly patients (79.5%), 5) increased interest in lifelong learning through additional training (67.3%), 6) increased interest in pursuing other postgraduate studies (49.0%), and 7) enhanced career opportunities (48.9%).
There were significant changes in the number of elderly patients seen per day by the respondents after the Course. The median of the range of elderly patients seen per day increased from 11-15 before the Course to 16-20 after the Course. Of the 43 respondents who were not on a fixed salary, the mean percentage of income contributed by caring elderly patients increased slightly from 24.2% to 27.6% after the Course.
While the majority of respondents had not conducted nursing home visit , there were significant increases in nursing home visits after the Course . The proportion of respondents who paid visits to nursing home increased from 19.8% to 28.1% after the Course. Most of them paid 1-5 visits to nursing home per month. Of the 69 (71.9%) respondents who did not conduct any home visit after studying the Course, they rated time constraint (39.7%) and limited job opportunities (38.4%) as the two main reasons. Other reasons included being limited by job nature/departmental policy (working in HA/GOPC) and did not know how to apply.
Respondents rated their confidence in diagnosing and managing common geriatric problems . Before the Course, only half of the respondents were confident of diagnosing (55.7%) and managing (51.6%) common geriatric problems such as dementia, falls, incontinence and stroke. After the Course, nearly all graduates were confident of diagnosing (98.9%) and managing (93.8%) common geriatric problems. The proportion of respondents strongly agreed to be confident increased greatly from 2% to over 30%.
For referral of elderly patients , the proportion of respondents being confident in deciding which specialty to refer to increased significantly from 73.1% to 94.6% after the Course. The percentage of respondents being strongly confident increased greatly from 5.4% to 35.5%. Most respondents did not refer elderly patients to private geriatricians, and would refer the patients to public geriatricians or other specialists. After the Course, the mean of the percentage of elderly patients being referred to private geriatricians increased from 2.8% to 6.1%, while to other specialists decreased from 53.4% to 49.1%. The average percentage of referrals to public geriatricians remained around 44%.
Regarding the coordination with social support services for elderly patients, 66.3% of respondents found it difficult before the Course. This situation reversed after the Course. 67.3% of the graduates agreed or strongly agreed they could coordinate easily with social support services. However, there was still one-third (32.6%) of graduates who expressed difficulty in this. Graduates were asked if they would like to work with chronically ill elderly patients . The combined percentage of agree and strongly agree increased from 68.5% to 88.5% after the Course.
When asked if they hoped caring for elderly patients to be the main part of their practice , only half (48.9%) of the respondents agreed or strongly agreed before the Course. The percentage increased to 62.8% after the Course. Almost all (97.9%) respondents were satisfied with this Course, and 95.9% would recommend it to other doctors. Increased confidence or knowledge in clinical practices was regarded as the most important impact of the Course. Expensive drugs/investigations, coordination with supporting services and time constraint were the major challenges or barriers for some graduates to implement what they have learned.
Conclusions
The results show that the Course is effective in improving graduates' confidence and attitudes in looking after elderly patients with common geriatric disorders. There are significant changes in the practice characteristics of the graduates after the Course, including the increased number of patients and cases handled in relation to geriatrics, improved confidence in making referral and increased average percentage of referrals to private geriatricians . However, it is observed that a rather large proportion of graduates encountered the problems of coordination with social services and conducting nursing home visits.
ii. Feedback from Graduates
Increased confidence/knowledge in clinical practices:
Structured program designed specifically for the need of primary care: very useful to improve my daily practice in managing elderly patients.
(2001 graduate)
Update clinical knowledge especially bedside training that helped increase my confidence. Not just the notes which I can easily find in textbook.
(2001 graduate)
Increased understanding of patient needs and social resources available to them:
The management of geriatric medical problems requires a comprehensive and multi-disciplinary approach. The role of family doctor is to coordinate the services provided by various medical specialties.
(2002 graduate)
Comments about the teaching method:
I found the content and discussion relevant to my daily clinical practice. I feel encouraged to find ways to improve my clinical work in the future.
(2001 graduate)
We had the chances to visit a Geriatric Day Hospital and visit some Old Age Home, and to attach to the Community Geriatrics Assessment Teams. This enabled us to have an overview on the local community geriatrics service.
(2003 graduate)
I learned from my classmates in my group because most of them are experienced doctors.
(2003 graduate)
Excellent teachers who demonstrate their clinical skills and knowledge during bedside teaching.
(2004 graduate)
Comprehensive, concise, good teacher and good cases for demonstration.
(2005 graduate)
I learned the importance of humanity in practice of geriatrics - treating patients as a person.
(2007 graduate)
Six months for clinical attachment was very important. It could help our memory. We could ask questions directly to our tutors. Compared with other postgraduate courses which had only one session for clinical attachment.
(2007 graduate)
iii. External Examiners Comments
As one of the early Course Advisors and External Examiners for the Postgraduate Diploma in Community Geriatrics and in view of my long association over 27 years with colleagues in the field of Geriatric Medicine in Hong Kong, I am delighted to note the continuing success of the diploma course.
Prof Brian Williams (2000-2002)
The diploma is a particularly exciting development in that it crosses boundaries between primary and secondary care, and also between public and private healthcare system. This wide remit is more than adequately covered in the curriculum and in the extensive 10 month teaching programme. Arrangements for supervision and attendance record-keeping are excellent.
Dr Stephen Allen 2003
We confirmed that we were wholly satisfied with the content of the written paper and would compliment the local examiners on their careful scrutiny of the performance of individual questions as part of the assessment and review of the exam.
The clinical part of the exam ran on two sites and in both the selection of patients and descriptors was highly appropriate for the purposes of the exam. The clinical areas available for the exam, including for the history taking/ethics scenarios, were highly satisfactory. The time-keeping and the exam related procedures ran with efficiency and thoughtfulness. The careful scrutiny of marking arrangements and the scoring regimen with respect to pass/fail cut offs reflected academic professionalism.
Dr William Primrose and Dr Alan McKenzie 2008
Publications
Publications
Lam TP, Chow RWM, Lam KF, Lennox IM, Chan FHW, Tsoi SLT. Evaluation
of the learning outcomes of a year-long postgraduate training course in
community geriatrics for primary care doctors. Archives of Gerontology and
Geriatrics. 21 June 2010.
http://www.ncbi.nlm.nih.gov/pubmed/20573410
Lam TP, Chow RWM, Lam KF, Lennox IM, Chan FHW, Tsoi SLT. Evaluative Study on Learning Outcomes of Postgraduate Diploma in Community Geriatrics. Family Medicine Unit, The University of Hong Kong. Report published June 2009.
Lam TP, Kong TK, Chan FHW, Wong CP. A postgraduate diploma course in community geriatrics for primary care doctors: experience of first three years. The Hong Kong Practitioner 2004; 26:441-446.https://www.hkcfp.org.hk/Upload/HK_Practitioner/2004/hkp2004vol26oct/discussion_paper.html
Conference presentations
Healthy ageing: A complete biopsychosocial health. Ninth Asia/Oceania Regional Congress of Gerontology and Geriatrics, Melbourne, Australia. Oct 2011.
Postgraduate Diploma in Community Geriatrics for Primary Care Doctors. Global Community Engaged Medical Education, Australia. October 2010
Evaluative Study on Learning Outcomes of Postgraduate Diploma in Community Geriatrics. Wonca Asia Pacific Regional Conference, Hong Kong. June 2009.
The setting up of a conjoint clinical examination for Diploma in Geriatric Medicine and Postgraduate Diploma in Community Geriatrics. Triennial Conference. Royal College of Physicians and Surgeons of Glasgow, UK. November 2008.
The setting up of a diploma course in community geriatrics for primary care doctors. The Royal Australian College of General Practitioners 45th Annual Scientific Convention. Australia October 2002.
The setting up of postgraduate diploma in community geriatrics at The University of Hong Kong. Inaugural Symposium of the Asian Medical Education Association, Hong Kong. June 2001.
Media Coverage
SC Allen. Hong Kong – ahead of the game. British Geriatrics Society Newsletter. January 2004.
社區健康防綫:一家庭,一醫生。香港經濟日報副刊。2001年10月11日。
Geriatric medicine improving with age. Medical Tribune. November 2002.
People
Board of Studies
|
Chairman: |
Prof Tai Pong Lam
|
|
Course Coordinator: |
Dr Chow Wai Man
|
|
External Examiner: |
Dr Angela Campbell
|
|
Members: |
Professor Gabriel M Leung
Prof Irene Ng
Prof Cindy Lam
|
|
Co-opted Members: |
Dr Felix Chan
Dr Daniel Chu
Dr Kong Tak Kwan
Dr Leung Man Fuk
Dr Lum Chor Ming
Dr Wong Chun Por
Dr Carolyn Kng
|
External Examiners
Professor Brian O Williams (2000 - 02)
MB ChB, MD, Hon DSc
Prof Williams, immediate Past President of the Royal College of Physicians and Surgeons of Glasgow, attained his MD in 1984 and has published over 130 original and review papers and 20 books or chapters on aspects of medicine in old age. He is also Chairman of the Federation of Royal Colleges of Physicians of the United Kingdom and Chairman of the Forum of the Royal Colleges of Surgeons and the Federation of Surgical Specialty Associations of Great Britain and Ireland (2007-2009). In 2008 he was awarded the Glasgow Lord Provost's Award in the category of Health.
Dr Stephen C Allen (2002 - 03)
MD, FRCP
Dr Allen is consultant physician and senior lecturer in General Medicine and Geriatrics, Royal Bournemouth & Christchurch Hospitals NHS Foundation Trust, Professor of Clinical Gerontology at Bournemouth University and former Chair of the Standards Advisory Committee for Geriatric Medicine, Joint Royal College of Physicians Training Board.
Dr Iain M Lennox (2003 - 07)
MBChB, MRCP, FRCP
Dr Lennox is Consultant Physician at the Medicine for the Elderly Directorate, South Glasgow Univerity Hospitals NHS Trust, UK. He has a broad-based interest in geriatric medicine and continuing care, and succeeded in a number of innovative projects including the establishment of a Stroke Rehabilitation Clinic and a Parkinson��s Disease Clinic, the first of its kind in Scotland. He has also produced over 20 publications in peer-reviewed journals.
Professor David J Stott (2005 - 07)
MBChB, MD, FRCP, MRCP
Prof Stott is David Cargill Professor of Geriatric Medicine, University of Glasgow and Honorary Consultant at the Academic Section of Geriatric Medicine, Royal Infirmary, Glasgow. He has conducted a broad portfolio of original research which involves national (Dundee) and international collaborations (Eire, Netherlands, Australia) and is directly relevant for healthcare of older people.
Dr William R Primrose (2007 - 09)
MBChB, MRCP, FRCP, MRCGP
Dr Primrose is Consultant Physician at the Department of Medicine for the Elderly, Woodend Hospital in Aberdeen, UK. He has delivered presentations on a wide range of topics related to geriatric diseases and continuing care, and has published over 40 journal articles and papers. His research interest includes the role and development of nursing home care, respite care, day hospital provision for geriatric patients.
Dr Alan K McKenzie (2007 - 08, 2009 - 11)
MBChB, MRCP
Dr McKenzie is Consultant Physician in geriatric medicine, Stirling Royal Infirmary in the UK. He takes a special interest in education and training, and has active participation in training, registrar and research work related to geriatric medicine. He has participated in a number of studies on multicentre and published on topics of common elderly diseases.
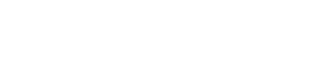
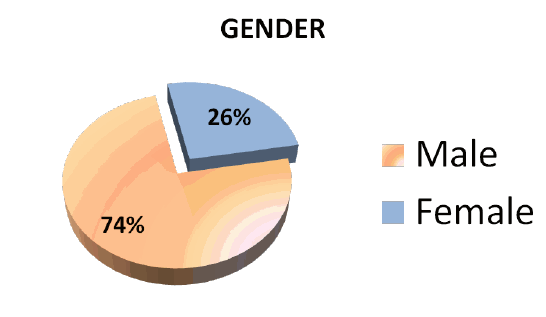
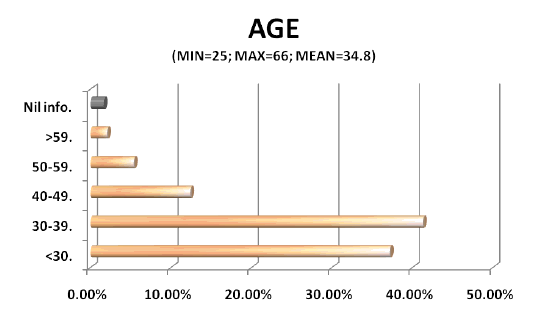
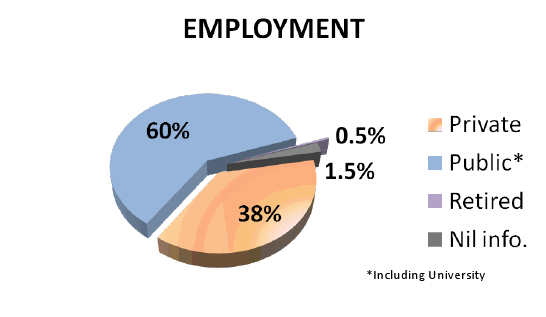
Student Profile
There is a total of 242 doctors enrolled in our Postgraduate Diploma in Community Geriatrics since 2000. The diagrams below show the general characteristics of our students.
N=242

Alumni Sharing
"The Postgraduate Diploma of Community Geriatrics is composed of lectures and clinical attachment. The lectures are delivered by very experienced geriatricians. In addition to the lecture notes, a textbook written by the local geriatricians is provided to the students. The contents are made relevant to diseases of elderly patients in Hong Kong. The clinical attachment provides excellent opportunities for learning geriatric medicine and clinical skills. On the whole, the course covers in depth those areas that are only barely touched upon in undergraduate curriculum.
After taking this course, I have become more capable of treating and managing elders both at my clinic, and in old age homes.
I strongly recommend this course to all primary care physicians."
Dr TSOI Lai To Sammy
(2002 Graduate)
"The knowledge i gained from the Course about common geriatric diseases helps improve my care for the geriatric patients. The clinical attachment is both rewarding and challenging.
I thank GOD for the privilege of being a doctor who can have chances to enhance my geriatrics knowledge. I believe it's the heart of a doctor and the attitude of learning which help shaping a better doctor."
Dr CHAN Yu Wesley
(2006 Graduate)