Postgraduate Diploma in Community Psychological Medicine (Sunsetted)
社區精神醫學深造文憑
This Course aims to help practising doctors understand more about the psychological nature of the problems that are troubling their patients and how to better manage them. Problems such as difficulty to falling asleep at night, chronic pain and headaches that are not due to a known illness, loss of interest in things, and shortness of breath, heart palpitations or shaking while at rest etc, have become more common and it is estimated that 25-40% of primary care consultations do carry a significant psychological component.
Since 2002, the Course has attracted over 230 doctors to further their training in psychological medicine. Not only have our graduates acquired greater confidence in treating patients with problems like the above, they have also recognised the need for early detection and appropriate referral of these patients to specialist care.
Developed jointly with the Department of Psychiatry, The University of Hong Kong, the Course employed different modes of study to facilitate interactive learning. These included seminars, group discussions of cases, clinical training sessions in psychotherapy and clinical teaching sessions by specialist clinicians. Clinical teaching was conducted at various clinics and public hospitals where the psychiatry teams were based. A postgraduate diploma was awarded upon satisfactory performance in the Course assessment and final examinations. Accreditations for CME, CPD and SEP points were applied upon completion of the Course.
Owing to the decreased enrollment numbers in recent years, our Department no longer offers admission to this Course which has therefore been sunsetted since 2017.
Features
- A Quotable Qualification by the Medical Council of Hong Kong
- Clinically Oriented
- Multiple Learning Modes
- Clinical Teaching Sites across Hong Kong
Objectives
Background
Patients presenting with psychological problems are frequently seen by primary care doctors. Most of these patients' problems are not serious in nature and will respond well to treatments by their primary care doctors if these are recognised and treated early. It is anticipated that the number of patients with psychological problems will continue to increase and comprise an even greater proportion of those seeking health services.
However, most of the primary care doctors practising today have little undergraduate training in the healthcare issues that are relevant to patients with psychological problems. The launch of a postgraduate course in this respect aimed to offer further and appropriate training for doctors who were interested and felt the need to enhance their skills and knowledge in the psychological medical care of their patients. It was expected that graduates of this Course would be able to look after most of their patients with psychological problems and be able to recognise those patients in need of specialist care for early referral
Objectives
- To promote the practice of psychological medicine among primary care doctors
- To improve the knowledge, skills and confidence of primary care doctors in the care of patients with psychological problems
- To emphasise the aspects of care that are different for patients with psychological problems
- To present information on the medical care of patients with psychological problems that is practical, concise and relevant to primary care
- To appreciate the interdisciplinary nature of psychological medicine
- To focus on community care, i.e. assessment of patients with psychological problems in their normal community environment, and the use of community resources as an integral part of their care
- To emphasise the importance of prevention and health maintenance in patients with psychological problems
- To present a positive model of psychological medical practice
Content & Schedule
Course Structure
| Seminar | Clinical Attachment | |
| Features | 20 seminars on topics related to common psychological problems with emphasis on their diagnoses and management |
5 Psychotherapy sessions 6 Clinical sessions including bedside teaching 2 Video review sessions 7 Case discussion sessions |
| Study Period | September - January the following year | January - June |
| Time | 20 Saturday afternoons (2:00-4:00 pm) | 20 weekday afternoons (2:00-4:00 pm) |
| Venue | Centrally located venue | Public hospitals/clinics |
| Assessment | Case report, written and clinical examination | |
Seminars
There were 20 seminars held on Saturday afternoons (2:00 - 4:00 pm). The seminars contained talks by experienced psychiatrists/clinical psychologists and case presentation by family physicians to facilitate active discussion.
*Seminar topics:
- Overview and interview skills
- Stress related disorders
- Panic and phobic disorders
- Obsessive-compulsive and related disorders
- Mood disorders including bipolar disorders
- Sleep disorders
- Eating disorders
- Sexual disorders
- Somatoform disorders
- Substance abuse including alcoholism
- Psychotic disorders
- Personality disorders
- Mental disorders in women
- Child and adolescent psychiatry
- Psychogeriatrics
- Basic psychopharmacotherapy
- Psychotherapy - behavioural
- Psychotherapy - cognitive-behavioural
- Consultation skills
- Crisis intervention and suicide
*Topics might be revised
Clinical Attachment
There were 20 clinical sessions held weekly from January-June at designated public hospitals or clinics where the psychiatric teams were based. Students were divided into small groups and attached to the teaching hospital of their choice. Each session lasted 2 hours and was led by a tutor (either psychiatrist or clinical psychologist from the hospital).
The 20 sessions contained 5 training sessions on psychotherapy conducted by clinical psychologists, 5 bedside teaching sessions and 8 case discussion sessions led by psychiatrists in which students presented their own patient cases for discussion. Two video review sessions were also carried out in primary care settings which enabled students to review and reflect on their own interviews with patients.
Case Report
Students were required to write one case report (around 2,000 words) as part of the continuous assessment.
Schedule and Venue
The Course commenced in September and finished in June the following year.
| Month | 9 | 10 | 11 | 12 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 |
| Seminars |
|
|||||||||||
| Clinical attachment |
|
|
||||||||||
| Case report |
|
|||||||||||
| Examinations | ||||||||||||
Teaching sites:
| Study Mode | Venue |
| Seminars | Duke of Windsor Social Service Building, 15 Hennessy Road, Wanchai, HK |
| Clinical Attachment | Students were assigned to attach to one of the following three groups: Kowloon 1, Kowloon 2 and New Territories. |
| Student Groups | Teaching Hospitals for clinical sessions |
| Hong Kong | Queen Mary Hospital |
| Kowloon 1 | Kowloon Hospital |
| Kowloon 2 | East Kowloon Psychiatric Clinic (in Diamond Hill) |
| New Territories | Castle Peak Hospital |
* Students were required to attend at least 80% of all the seminars and clinical sessions in order to fulfill the requirements for the award of the diploma.
Assessment & Awards
Assessment
The performance in written assignment and clinical sessions provided continuous assessment. There were also final examinations with a written paper and a clinical oral examination. Examiners comprised family physicians and psychiatrists. Local and/or external examiner(s) were invited to participate in the final examinations.
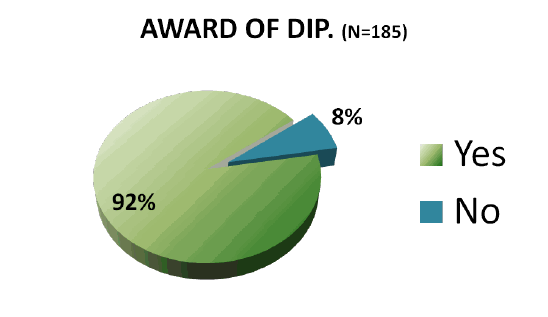
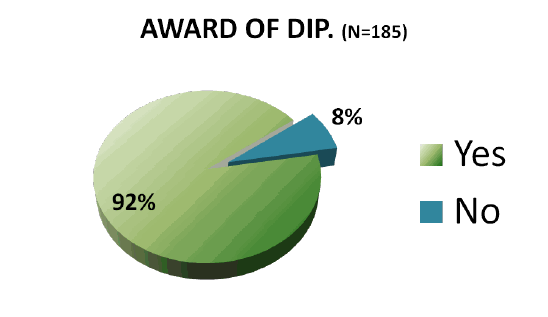
Award of Diploma
The Postgraduate Diploma in Community Psychological Medicine was awarded to the candidates who completed the whole Course and performed satisfactorily in the Course assessment and final examinations. The Diploma is recognized as a quotable qualification by the Medical Council of Hong Kong.
Accreditations for CME, CPD and SEP points were applied to the Colleges of the Hong Kong Academy of Medicine, Department of Health, Hong Kong Medical Association and Hong Kong Doctors Union.
Learning Outcomes
i Learning Outcomes
An evaluative study on the learning outcomes of the Postgraduate Diploma in Community Psychological Medicine graduates was carried out in 2008 and a report on the findings was published in 2009.
Background
There is an increasing worldwide trend to strengthen the quality of primary care doctors by further postgraduate studies. Although overseas experiences have indicated improvements in doctors’ clinical practice and other areas after taking postgraduate courses, little is known about the possible effect of these courses in enabling doctors to handle cases which would reduce burden of specialists and their participation in more demanding community healthcare activities. The present study aims to fill the gap in this respect and has selected the Postgraduate Diploma in Community Psychological Medicine (PDCPM) as its main subject. The PDCPM, developed by the Family Medicine Unit and Department of Psychiatry, The University of Hong Kong, has trained over 140 primary care doctors since 2003.
Aims
1. To examine the learning outcomes of the PDCPM, including improvement in clinical skill, patient care and participation in community healthcare
2. To document the practice characteristics of the graduates before and after the Course, including the number of patients and cases handled in relation to the course subject, level of confidence and the percentage of referral to psychiatrists
3. To examine the doctors’ expectations of postgraduate studies, and the long-term effect upon graduation, e.g. lifelong learning and updating of medical knowledge, initiative in further contribution to community heathcare
Methods
A questionnaire designed by the research team was sent to all graduates (2003-2007) of the PDCPM between August and December 2008 after its pilot test in mid-July of the same year. To enhance the response rate, three rounds of invitation were sent followed by telephone reminders. The questionnaire itself was anonymous but was coded with a reference number to identify the respondent for the lucky draw prizes or for deletion from the next round of invitation.
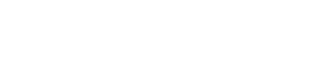
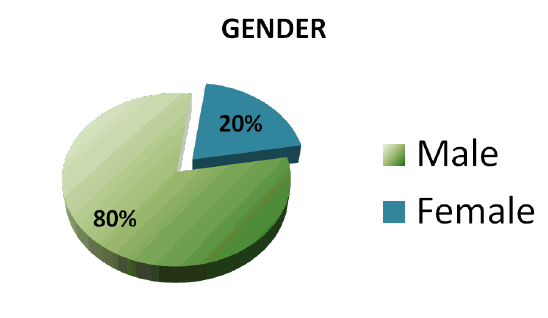
Results
Out of the 118 questionnaires sent to the graduates, we have received 69 replies after three rounds of invitation, with a response rate of 58.5% (69/118). Of the respondents, 80.9% were male and 19.1% female, 95.6% were in community practice while 4.4% in hospital practice, 88.4% were in private service and 11.6% were in public service. A great majority (95.7%) of the respondents were primary care doctors, and the mean years after graduation from medical school was 19.5±9.01.
The respondents rated the reasons for studying the Course in descending order of importance: 1) improve care for patients with mental health problems (100.0%), 2) update clinical knowledge (98.5%), 3) interest in community psychological medicine (97.0%), 4) lifelong learning (94.1%), 5) acquire qualifications (86.8%), 6) career enhancement (75.3%), 7) meet job demand (72.0%), and 8) CME accreditations (44.9%).
The rated major learning outcomes, in descending order of agree?ment, were: 1) increased confidence of discussing mental health problems with patients (100.0%), 2) increased understanding of the patients’ experience (98.6%), 3) improved knowledge of psychological treatment (97.1%), 4) modification of approach to patients (97.1%), 5) paid more attention to patients with mental health problems (95.7%), 6) improved knowledge of drug therapy for patients (94.2%), 7) increased empathy towards patients (94.2%), 8) reduced stereotyping of mental health problems (92.8%), 9) increased interest in lifelong learning through additional training (82.6%), 10) increased affiliation with societies of mental health (75.0%), 11) enhanced career opportunities (66.7%), and 12) increased interest in pursuing other postgraduate studies (63.7%).
There were significant changes in the number of patients whose chief complaint and associated symptoms were obviously psychological or psychosomatic seen per week by the respondents after the Course. The median of the range of these patients seen per week increased from 3-6 before the Course to 7-10 after the Course. Of the 43 respondents who were not on a fixed salary, there were significant increases in the percentage of income contributed by seeing these patients after the Course.
Respondents rated their confidence in diagnosing and managing common mental health problems. Before the Course, about half of the respondents were confident of diagnosing (50.0%) and managing (50.7%) common mental health problems such as anxiety, depression, dementia and insomnia. After the Course, almost all graduates were confident of diagnosing (96.9%) and managing (97.0%) common mental health problems. The proportion of respondents strongly agreed to be confident increased greatly from nearly none before the Course to around 55% after the Course.
We also asked the graduates about the time sufficiency to treat patients with common mental health problems. The proportion of respondents having enough time in their practice to treat patients with mental health problems increased from 55.8% to 72.1% after the Course.
For referral of patients with mental health problems, the proportion of respondents being confident of deciding which specialty to refer to increased from 72.8% to 97.0%. The proportion of respondents strongly agreed to be confident increased greatly from 6.1% to 48.5%. The number of referrals made by respondents to psychiatrists had dropped after the Course. Most respondents (76.6%) would refer not more than one-fifth of patients with mental health problems to psychiatrists after the Course, compared to 50.0% before the Course.
For the coordination with social support services with mental health problems, the proportion of respondents found it easy increased from 42.6% to 66.2% after the Course. However, there was still one-third (33.8%) of graduates expressing difficulty in this.
Regarding the attitudes towards taking care of mentally ill patients, only one-third (35.3%) of the respondents hoped caring for patients with mental health problems to be the main part of their practice before the Course. This percentage increased to 60.3% after the Course.
Almost all (98.5%) respondents were satisfied with this Course, and 95.6% would recommend it to other doctors. Increased confidence or knowledge in clinical practices, and modification of the approach to patients with mental health problems were considered as the most important impact of the Course. Time constraint and expensive drugs/investigations were the major challenges or barriers for some graduates to implement what they have learned.
Graduates were asked if they want to take short modular courses on specific topics of Psychological Medicine in the future. 64 respondents (92.8%) answered “Yes”. The top three topics being rated were psychotherapy (75.0%), child and adolescent disorders (46.9%) and psychopharmacology (40.6%).
Conclusion
The results show that the Course is effective in improving graduates’ confidence and attitude in looking after patients with common mental health problems. There are significant changes in the practice characteristics of the graduates after the Course, including increased number of patients and cases handled in relation to mental health problems, increased time sufficiency for consultation, increased confidence in making referrals to psychiatrists as well as decreased percentage of patients being referred.
ii. Feedback from Graduates
Increased confidence/knowledge in caring for patients with mental health problems:
Very useful course for updating and refreshing knowledge and skills in managing patient with mental health problems at primary care level.
(2004 graduate)
Being able to come to a diagnosis and management plan quickly and effectively and to know which cases need early referral to specialists.
(2005 graduate)
More confident of making the diagnosis, and more concrete and precise in history taking to elicit relevant symptoms of various mental disease.
(2005 graduate)
Increase exposure to common mental problems and increase expertise, better liaison with some psychiatrists and psychologists.
(2006 graduate)
Modification of their approach to patients:
Change my practice of seeing patients with unexplained medical/ somatic complaints to a more patient-oriented and psychological approach.
(2004 graduate)
Accepting psychiatric conditions as a manifestation of underlying endocrinologic derangement, not too much different from malfunctioning of the pancreas in diabetes.
(2005 graduate)
Psychological illness is much more common than I think. Early disease recognition and treatment makes a big difference to the patient’s sufferings.
(2005 graduate)
Improve communication with patients by empathy and sympathy. Happy to deal with mental illness and with less bewilderment.
(2007 graduate)
Able to see patients interviewed by psychiatrist during clinical attachment; reshape my approach to common psychiatric illness; certainly, better management then.
(2007 graduate)
Self development
It really opened up my mind, changed my attitude and to a moderate degree, my own personality and behaviour, not only in clinical practice, but also in private life.
(2004 graduate)
iii. External Examiners' Comments
It was a great privilege to be invited to be external examiner for the Post Graduate Diploma in Community Psychological Medicine. I found that the examinations were conducted seriously and with rigor and that the deliberations of the examiners were profound. Most of all I was impressed by the high standard of the candidates who graduated.
Professor Gavin Andrews 2011
In the time I have been an Examiner I have seen this Diploma strengthen, and provide new opportunities to family doctors in Hong Kong. The course that leads up to it is now well-established, and is beginning to be sought by physicians in other disciplines. I am grateful to my colleagues in Family Medicine for their openness to new ideas and for their hospitality and friendship, and to the University of Hong Kong for having provided me with the opportunity to assist in this important project.
Professor Sir David Goldberg 2009
Conference & Publications
Conference
2006 International Forum on Community Psychological medicine (IFCPM) -
Multidisciplinary Approach to Mental Healthcare
http://www.ifcpm.hku.hk/index.htm
A platform-building initiative guided by the theme of 'multidisciplinary approach to mental healthcare', the IFCPM attracted nearly 250 professionals from different disciplines including primary care doctors, psychiatrists, clinical psychologists, nurses, social workers and occupational therapists to participate in the four-day conference and workshops held from October 7 - 10, 2006.
The Family Medicine Unit (now renamed as Department of Family Medicine and Primary Care), joining hands with the Department of Psychiatry, The University of Hong Kong; Hong Kong Medical Association; and Hong Kong Community Psychological Medicine Association, together brought this initiative into fruition. Prominent scholars from overseas and the Mainland as well as numerous local professionals had also contributed their views and expertise on issues related to community psychological medicine.
The intense exchange and discussion during the conference demonstrated the bold steps taken by the participants to forge a multidisciplinary perspective and practice approach to mental healthcare - an important theme that translated into a position statement endorsed by participating organisations and public healthcare authorities at the IFCPM. The Forum ended with a public lecture with a full-house audience of 300.
Publications
Lam TP, Goldberg D, Tse EYY, Lam KF, Mak KY, Lam EWW. What do primary care doctors get out of a year-long postgraduate course in community psychological medicine? The International Journal of Psychiatry in Medicine. 2011; 42(2):133-149. http://baywood.metapress.com/index/X147127M1X01684L.pdf
Lam TP, Tse YY, Lam KF, Mak KY, Goldberg D, Lam WW. Evaluative Study on Learning Outcomes of Postgraduate Diploma in Community Psychological Medicine. Family Medicine Unit, The University of Hong Kong. Report published September 2009.
Lam TP, Lam KF, Tse EYY. Why do primary care doctors undertake postgraduate diploma studies in a mixed private/public Asian setting? Postgraduate Medical Journal. 2006; 82:400-403. http://pmj.bmj.com/content/82/968/400.abstract
Conference Presentations
The biopsychosocial approach in primary care - can it be taught to practicing primary care doctors?. Plenary Lecture. Family Medicine and Primary Care Symposium. Hong Kong. November 2011.
Five-year experience of a postgraduate diploma Course in psychological medicine. 13th Ottawa International conference on Clinical Competence, Melbourne, Australia. March 2008.
Factors affecting primary care doctors' decision to undertake postgraduate diploma studies. 11th Medical Research Conference, The University of Hong Kong. January 2006.
The setting up of a diploma course in community psychological medicine for primary care doctors. Wonca Asia Pacific Conference, Beijing, China. October 2003.
People
Board of Studies
|
Chairman: |
Prof Tai Pong LAM
|
|
Course Coordinator: |
Dr Dawn Ai
|
|
External Examiner: |
Dr Chou Yuan Hwa
|
|
Members: |
Professor Gabriel M Leung
Prof YF Cheung
Prof Cindy Lam
Prof E.Y.H. Chen
Prof Mak Ki Yan
Dr Ronald Chen
|
|
Co-opted Members: |
Dr Lo Tak Lam
Dr Desmond Nguyen
Dr Bonnie Siu
|
External Examiners
Professor Sir David Goldberg (2002 - 2009)

Professor Goldberg, MSc, MD, FRCP, FRCPsych, is Professor Emeritus at the Institute of Psychiatry, King's College. He is an Honorary Fellow of the Royal College of Psychiatrists and a Fellow of the Academy of Medical Sciences. Being a pioneer in the field of primary mental health care since the mid-1960s, Professor Goldberg is internationally renowned for his great contribution and enthusiasm in supporting research and education in this field worldwide, including Hong Kong. Professor Goldberg directed the World Psychiatric Association project of Training Primary Care Staff in Mental Health Skills. He is the author of the General Health Questionnaire and the Clinical Interview Schedule which have been widely used across the world.
Professor Gavin Andrews (2009 - 2010)

Prof Andrews, MB, ChB, MD, DipPsyMed, FRANZCP, FRCPsych, from the School of Psychiatry, University of New South Wales, is internationally renowned for his enthusiasm and contribution to research and education activities in the field of psychological medicine. He is distinguished in his design and implementation of Australia's only national mental health survey. His research team has also developed expertise in calculating the cost effectiveness of treatments for ten mental and three physical disorders. Moreover, he is also expert in an active program of internet treatment of anxiety and depressive disorders in primary and specialist care.
Student Profile
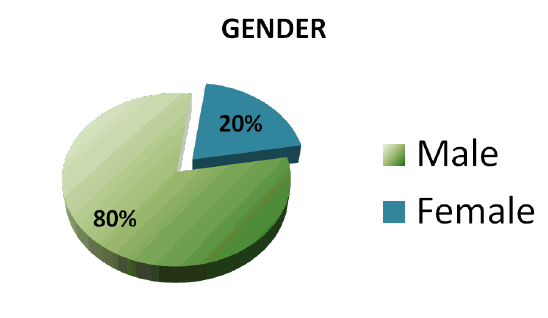
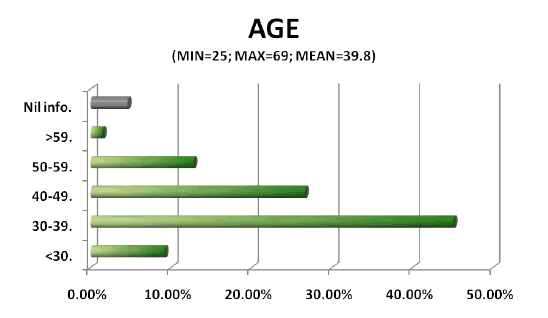
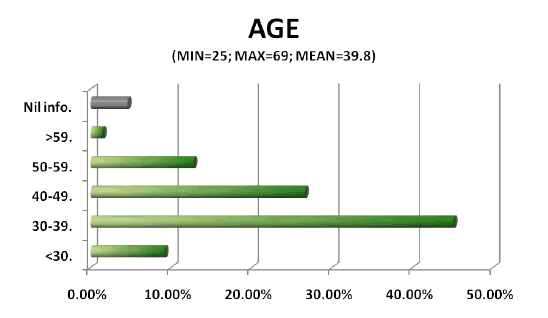
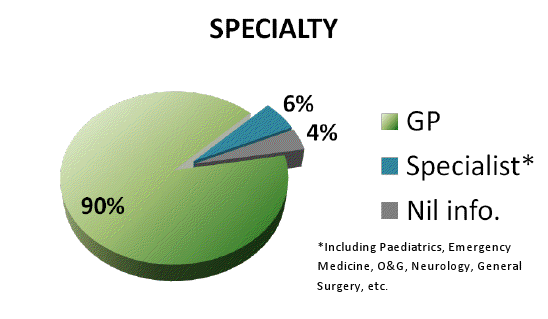
There is a total of 195 doctors enrolled in our Postgraduate Diploma in Community Psychological Medicine since 2002. The diagrams below show the general characteristics of our students.
N=195


Alumni Sharing
"As a primary care doctor, I found attending the Postgraduate Diploma in Community Psychological Medicine extremely practical and helpful in the following ways:
1: building up and maintaining rapport with all types of patients, including the most challenging one
2: sharpening my ability to approach patients with the bio-psycho-social approach (not limited to those with predominant psychiatric problems), which often result in better doctor and patient satisfaction and therapeutic efficacy
3: develop a most up-to-date understanding of commonly encountered psychological problems and psychiatric disorders in primary care and their management at primary care level
4: more confident in managing common psychiatric disorders (increase comfort level) as well as becoming more aware of my limitations and when to refer
5: nurture my interest and enthusiasm in the fascinating field of neuro-biology and its application in primary care which make daily clinical work much more interesting
I have no hesitation in recommend this Course to all primary care doctors who desire to enhance their clinical skills in holistic care as well as enjoying clinical practice at a deeper level."

Dr TAM Chi Wing Peter
(2003 Graduate)
"While technological advancements have enhanced medical care significantly, mental health problems remain to be underpresented, underdetected and undertreated in the community. In the 21 st century, everybody deserves to be cared by doctors who can appreciate the complexity of human sufferings, assess health problems biopsychosocially, provide quality psychological care and use medications rationally. The diploma course has been designed to empower you to face these challenges. I have become a happier and more competent doctor through taking this course. Graduates have formed an association for supporting continuous professional development, research and collaboration with other mental health professionals. I strongly recommend this Course to all doctors. It will be a turning point to your career. Your effort will not be wasted."

Dr LAM Wing Wo Edmund
(2004 Graduate)
"Medicine is about the mind, the body and the interaction in between. More than 90% of our prior training concentrated on the pathophysiological process of the human body. Naturally, when dealing with mental patients, we either keep a blind eye to these patients or simply talked the problem down and pacify the patient with ineffective strategies. In either way, the patient and the doctor suffer. The patient has an unsatisfactory treatment encounter; the doctor has a defeat in his/her healing career."
"For ways to better the management, I heartily recommend the Postgraduate Diploma in Community Psychological Medicine to any doctor who believes in holistic medicine. One will be facilitated through a new clinical dimension by a systematic course, practical teaching and friendly staff. Students learn new therapeutics, aware of their limits and serve a triage link to the secondary specialist care. The potential gain is only limited by one's own input. Indeed, one of the most fruitful years in my 24 years of continuous medical education."

Dr CHAN Suen Ho Mark
(2005 Graduate)
Conference & Publications
Conference
2006 International Forum on Community Psychological medicine (IFCPM) -
Multidisciplinary Approach to Mental Healthcare
http://www.ifcpm.hku.hk/index.htm
A platform-building initiative guided by the theme of 'multidisciplinary approach to mental healthcare', the IFCPM attracted nearly 250 professionals from different disciplines including primary care doctors, psychiatrists, clinical psychologists, nurses, social workers and occupational therapists to participate in the four-day conference and workshops held from October 7 - 10, 2006.
The Family Medicine Unit (now renamed as Department of Family Medicine and Primary Care), joining hands with the Department of Psychiatry, The University of Hong Kong; Hong Kong Medical Association; and Hong Kong Community Psychological Medicine Association, together brought this initiative into fruition. Prominent scholars from overseas and the Mainland as well as numerous local professionals had also contributed their views and expertise on issues related to community psychological medicine.
The intense exchange and discussion during the conference demonstrated the bold steps taken by the participants to forge a multidisciplinary perspective and practice approach to mental healthcare - an important theme that translated into a position statement endorsed by participating organisations and public healthcare authorities at the IFCPM. The Forum ended with a public lecture with a full-house audience of 300.
Publications
Lam TP, Goldberg D, Tse EYY, Lam KF, Mak KY, Lam EWW. What do primary care doctors get out of a year-long postgraduate course in community psychological medicine? The International Journal of Psychiatry in Medicine. 2011; 42(2):133-149. http://baywood.metapress.com/index/X147127M1X01684L.pdf
Lam TP, Tse YY, Lam KF, Mak KY, Goldberg D, Lam WW. Evaluative Study on Learning Outcomes of Postgraduate Diploma in Community Psychological Medicine. Family Medicine Unit, The University of Hong Kong. Report published September 2009.
Lam TP, Lam KF, Tse EYY. Why do primary care doctors undertake postgraduate diploma studies in a mixed private/public Asian setting? Postgraduate Medical Journal. 2006; 82:400-403. http://pmj.bmj.com/content/82/968/400.abstract
Conference Presentations
The biopsychosocial approach in primary care - can it be taught to practicing primary care doctors?. Plenary Lecture. Family Medicine and Primary Care Symposium. Hong Kong. November 2011.
Five-year experience of a postgraduate diploma Course in psychological medicine. 13th Ottawa International conference on Clinical Competence, Melbourne, Australia. March 2008.
Factors affecting primary care doctors' decision to undertake postgraduate diploma studies. 11th Medical Research Conference, The University of Hong Kong. January 2006.
The setting up of a diploma course in community psychological medicine for primary care doctors. Wonca Asia Pacific Conference, Beijing, China. October 2003.
People
Board of Studies
|
Chairman: |
Prof Tai Pong LAM
|
|
Course Coordinator: |
Dr Dawn Ai
|
|
External Examiner: |
Dr Chou Yuan Hwa
|
|
Members: |
Professor Gabriel M Leung
Prof YF Cheung
Prof Cindy Lam
Prof E.Y.H. Chen
Prof Mak Ki Yan
Dr Ronald Chen
|
|
Co-opted Members: |
Dr Lo Tak Lam
Dr Desmond Nguyen
Dr Bonnie Siu
|
External Examiners
Professor Sir David Goldberg (2002 - 2009)

Professor Goldberg, MSc, MD, FRCP, FRCPsych, is Professor Emeritus at the Institute of Psychiatry, King's College. He is an Honorary Fellow of the Royal College of Psychiatrists and a Fellow of the Academy of Medical Sciences. Being a pioneer in the field of primary mental health care since the mid-1960s, Professor Goldberg is internationally renowned for his great contribution and enthusiasm in supporting research and education in this field worldwide, including Hong Kong. Professor Goldberg directed the World Psychiatric Association project of Training Primary Care Staff in Mental Health Skills. He is the author of the General Health Questionnaire and the Clinical Interview Schedule which have been widely used across the world.
Professor Gavin Andrews (2009 - 2010)

Prof Andrews, MB, ChB, MD, DipPsyMed, FRANZCP, FRCPsych, from the School of Psychiatry, University of New South Wales, is internationally renowned for his enthusiasm and contribution to research and education activities in the field of psychological medicine. He is distinguished in his design and implementation of Australia's only national mental health survey. His research team has also developed expertise in calculating the cost effectiveness of treatments for ten mental and three physical disorders. Moreover, he is also expert in an active program of internet treatment of anxiety and depressive disorders in primary and specialist care.
Student Profile
There is a total of 195 doctors enrolled in our Postgraduate Diploma in Community Psychological Medicine since 2002. The diagrams below show the general characteristics of our students.
N=195


Alumni Sharing
"As a primary care doctor, I found attending the Postgraduate Diploma in Community Psychological Medicine extremely practical and helpful in the following ways:
1: building up and maintaining rapport with all types of patients, including the most challenging one
2: sharpening my ability to approach patients with the bio-psycho-social approach (not limited to those with predominant psychiatric problems), which often result in better doctor and patient satisfaction and therapeutic efficacy
3: develop a most up-to-date understanding of commonly encountered psychological problems and psychiatric disorders in primary care and their management at primary care level
4: more confident in managing common psychiatric disorders (increase comfort level) as well as becoming more aware of my limitations and when to refer
5: nurture my interest and enthusiasm in the fascinating field of neuro-biology and its application in primary care which make daily clinical work much more interesting
I have no hesitation in recommend this Course to all primary care doctors who desire to enhance their clinical skills in holistic care as well as enjoying clinical practice at a deeper level."

Dr TAM Chi Wing Peter
(2003 Graduate)
"While technological advancements have enhanced medical care significantly, mental health problems remain to be underpresented, underdetected and undertreated in the community. In the 21 st century, everybody deserves to be cared by doctors who can appreciate the complexity of human sufferings, assess health problems biopsychosocially, provide quality psychological care and use medications rationally. The diploma course has been designed to empower you to face these challenges. I have become a happier and more competent doctor through taking this course. Graduates have formed an association for supporting continuous professional development, research and collaboration with other mental health professionals. I strongly recommend this Course to all doctors. It will be a turning point to your career. Your effort will not be wasted."

Dr LAM Wing Wo Edmund
(2004 Graduate)
"Medicine is about the mind, the body and the interaction in between. More than 90% of our prior training concentrated on the pathophysiological process of the human body. Naturally, when dealing with mental patients, we either keep a blind eye to these patients or simply talked the problem down and pacify the patient with ineffective strategies. In either way, the patient and the doctor suffer. The patient has an unsatisfactory treatment encounter; the doctor has a defeat in his/her healing career."
"For ways to better the management, I heartily recommend the Postgraduate Diploma in Community Psychological Medicine to any doctor who believes in holistic medicine. One will be facilitated through a new clinical dimension by a systematic course, practical teaching and friendly staff. Students learn new therapeutics, aware of their limits and serve a triage link to the secondary specialist care. The potential gain is only limited by one's own input. Indeed, one of the most fruitful years in my 24 years of continuous medical education."

Dr CHAN Suen Ho Mark
(2005 Graduate)